For health professionals working in the NHS, providing appropriate advice and support for children with ASD or ADHD is just as complex.
They too must steer a delicate course between what the published evidence tells them, and what they feel the individual needs of the child in front of them might be. As if that’s not enough, they must then balance all of this with the child’s parent’s perception of need.
The parent will be able to draw on hundreds of observations about what their child eats and whether or not this is affecting their health and wellbeing.
Health professionals and parents working together
Both parent and health professional will often bring with them a degree of bias and prejudice about the likely impact of diet. The health professional might argue that they are better trained to evaluate the quality and relevance of scientific research papers. The parent might argue that they have more experience of how their child is affected by food. Sometimes they might even dare to suggest that they have read more of the research and are better informed than the health professional! The seeds of conflict can be quickly sown, and if the relationship between the parents and health professionals break down, the child may be the one who suffers the most.
Traditional health professional/patient (or parent) relationships have been quite paternalistic in nature. The Health Professional has the expertise, decides what treatment is most appropriate, and prescribes this accordingly.
The more progressive health professional accepts that patients and their parents or carers should be involved in decision-making. It can be difficult to know where to stop, however. If we are to ensure both the safety of the child, and the most effective use of limited resources, health professionals should not simply cave in to every demand. This would be a “consumerist” healthcare model which can be more dangerous and inequitable than a traditional one.
"Health policy should be based on a rational assessment of all the evidence available."
Rational, logical analysis has served health professionals and scientists well over the years. Health policy should be based on a rational assessment of all the evidence available. In order to do this, we have rules that govern what constitutes a good “level of evidence”. For example, the incidence of strokes was once very high in Finland. Finnish is not extensively spoken in any other country.
Analysis merely of the statistics might conclude that speaking Finnish is a cause of strokes. Common sense tells us that this is not very likely. If common sense is not enough, we can design a clinical trial to prove or disprove that speaking Finnish causes the incidence of strokes to rise. In this way, we can distinguish between a coincidence (chance), a consistent correlation, and cause and effect (where speaking Finnish actually causes strokes). We used to think that, for example, eating cholesterol was a major cause of heart disease until clinical trials showed that this was not the case.
The “gold standard” for evidence comes from clinical trials that are “blinded” and “placebo controlled” with large subject numbers and treatment effects. If several such clinical trials all point in the same direction, the intervention is likely to be recommended by groups such as NICE (National Institute for Clinical Excellence) or SIGN (Scottish Intercollegiate Guideline Network). Indeed, guidelines on ASD and ADHD are published by such bodies and include, with varying degrees of rigour, an attempt to grapple with nutritional interventions.
Unfortunately, there are very few well designed trials on diet and ASD or ADHD. No wonder then that NICE and SIGN are hardly enthusiastic in their review of nutritional approaches. Let us leave aside for one moment, the specifics of ASD and ADHD. Commercial and practical constraints mean there are substantial barriers to nutrition research per se, with drugs trials being easier to fund and design than nutrient trials, and nutrient ones being easier than those involving real foods or whole diets. If we based our public health nutrition policy only on the analysis of blinded, placebo controlled trials, what would we be recommending as the cornerstones of a healthy diet?
Real food already exists in nature. As such, it has very little patentable value and therefore research on its effect on health is not as attractive to would-be funders when compared with drugs, supplements or “functional foods”. It is also difficult to design a blinded study involving real food as the participant usually knows what they are eating! One can design a blinded placebo controlled trial of a specific substance, but what about whole foods? What about whole diets? The public health message becomes: “Don’t bother with eating more fish, fruits and vegetables, just eat more Benecol, and keep taking the drugs”. The box below shows the 5 questions that, I believe, should be asked before a dietary intervention can be seriously considered:
Five questions to help evaluate the suitability of dietary intervention for ASD and ADHD
1. Are there
plausible mechanisms through which the nutrient, food or diet might help?
2. Is there
some
evidence from
clinical trials in favour of the nutrient, food or diet?
3. Is there evidence of marginal or excessive intakes
at the population level?
4. Is the food, nutrient, or diet broadly consistent with
“healthy eating” messages?
5. Are there
populations
who consume this nutrient, food or diet at this level,
without
obvious
harmful effects?
For drugs and other medical interventions, only the first two questions are relevant.
The other three questions can only be applied to diet.
Some interventions will score more strongly on some points than others.
In particular, question 3 is vital. There is evidence that, as a population, we eat far too much saturated fat, added sugar and salt and not enough fruit, vegetables and oily fish.
"Is it plausible that the brain is not affected?"
While the understanding of how this kind of modern diet affects the brain is still in its infancy, we know it affects physical health. Is it plausible that the brain is not affected?
Our default position – our assumption, unless there is clear evidence to the contrary, should be that we should strive to address this imbalance for each individual child with ASD or ADHD. The benefits may be physical, mental or cognitive; and noticeable in the short, medium or long term.
We should also briefly consider what we mean by “help
children with ASD or ADHD”. We are rightly suspicious of “therapists” who promise to “cure” Autism. Autism is not curable and many people with such a diagnosis would not want to be “cured” anyway. However, it is clear that children with an ASD or ADHD diagnosis are often more vulnerable to difficulties in mood, behaviour, learning and sleep.
Those with a poor diet (more common in ASD) are also more vulnerable to long term diet-related illness such as cancer, stroke, obesity and heart disease. Some researchers have suggested that metabolic differences mean a higher proportion of children with ASD or ADHD are more vulnerable to “oxidative stress”. If this is true, it further adds to the importance of a good diet rich in “antioxidants” and nutrients that may be particularly prone to oxidation (such as omega 3 fats).
Applying these 5 questions, some specific dietary approaches stand out as being sensible, safe and possibly effective. These will, no doubt, change as further evidence accumulates. Those that I would currently recommend are shown at the end of this paper. These interventions should be considered as a menu of treatment options between health professional, parent and child. In doing so, we can have new health professional/parent relationships, based on shared decision-making, rather than the two extremes of paternalistic or consumerist models of healthcare.
"Health professionals should see the motivation of parents to find the right diet for their child as an opportunity, not a threat."
There is considerable concern, by NHS health professionals about families seeking
alternative
sources of care and advice. However, if we can engage families in a sensible discussion about diet, health and wellbeing using these rules as a starting point, families would be less inclined to seek out these sources. There are some who will always be looking to go to the “next level”, those who will leave “no stone unturned”. However, my experience of working with families in Highland, tells me that the vast majority accept their child’s diagnosis, and just want to ensure that their diet is as conducive to physical, mental and emotional good health as possible.
If the evidence about the impact of diet on brain function is rather weak and patchy, then we should be honest enough to say so. But families should feel encouraged and supported in their attempts to improve their child’s diet. This is particularly important given that children with ASD or ADHD are often (but not always) at the poor end of an unhealthy modern food culture that is already less than healthy.
Health professionals should see the motivation of parents to find the right diet for their child as an opportunity, not a threat. It is obvious that parents of children who have a neuro-developmental diagnosis, will want to do everything they can to create the best possible conditions for good mood, behaviour and learning. Many will, therefore, have a healthy interest in diet and brain function. They will need support from well informed health professionals that can make general healthy eating guidelines relevant for their child. It is hoped that these rules provide a framework that enables health professionals to do just that.
A menu of dietary and nutritional recommendations for children with ASD and / or ADHD, with a view to safety, general healthy eating advice, and possible benefit in brain functioning
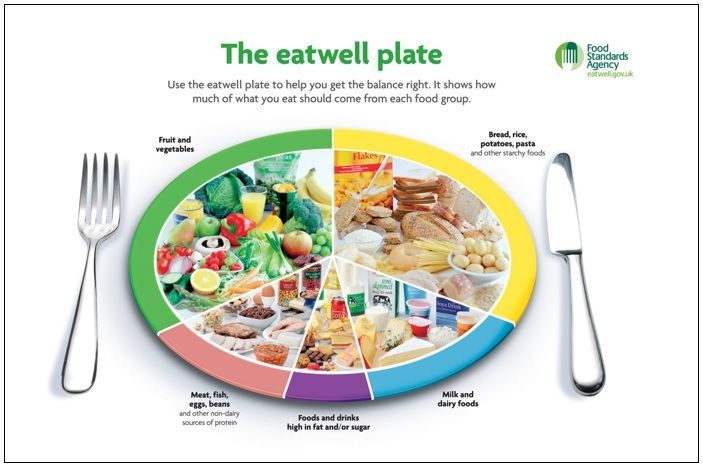
- Promotion of a “balanced diet” based on the
5 food groups as shown in the “Eatwell Plate”
- Eating regularly and not skipping breakfast
- Eating at least 5 potions of
fruit and vegetables a day (for folate, magnesium, antioxidants in general and fibre)
- Reduction in soft drinks /confectionery containing specific artificial food colours / benzoate preservatives (added benefit of reducing empty calories)
- Consideration and possibly testing of
vitamin D status with oral supplements for northerly latitudes, dark skin or indoor lifestyle
- Eating
oil rich fish or taking omega 3 supplements
- For those with an inadequate diet, the use of a multi-purpose
vitamin and mineral supplement where no ingredients exceed the reference nutrient intake
- Measurement of Ferritin stores and prescription of
Iron supplements depending on results
- Ensuring the inclusion of
Iron and Zinc rich foods or using supplements
- Consideration of
food intolerances to a range of foods through trial and error but only under the
supervision
of a State Registered Dietitian
Additional Supporting Healthy Messages from the FSA:
Bread, rice, potatoes, pasta and other starchy foods
Eat plenty, choose wholegrain varieties when you can
Fruit and vegetables
Eat plenty, at least five portions of a variety of fruit and vegetables a day.
Milk and dairy foods
Eat some, choose lower fat alternatives whenever possible or eat higher fat versions infrequently or in smaller amounts.
Meat, fish, eggs, beans and other non-dairy sources of protein
Eat some, choose lower fat alternatives whenever possible or eat higher fat versions infrequently or in smaller amounts. Aim for at least two portions of fish a week, including a portion of oily fish.
Foods and drinks high in fat and/or sugar
Eat just a small amount.
Try to choose options that are lower in salt when you can. Adults should have no more than 6 grams of salt a day.
David Rex explains there is no “one-size-fits-all’ when it comes to children’s nutrition and diet.
David Rex's Speaking Event(s)
For further insight from David Rex, Specialist Dietician, NHS Highland, listen to our FAB webinar events - available to download now.
June 11, 2024
What parents and professionals can do in practice to help children eat better - and to support their mental as well as physical health, wellbeing and performance
May 14, 2024
What Works, What Matters? Practical Solutions for Dietary Difficulties in ADHD, Autism and Related Conditions
September 28, 2023
How children's diets affect their health, wellbeing and performance - and what parents, professionals and policymakers can do to help
January 25, 2023
Find out what the latest research shows about selective / avoidant eating in children, and its possible causes and consequences.